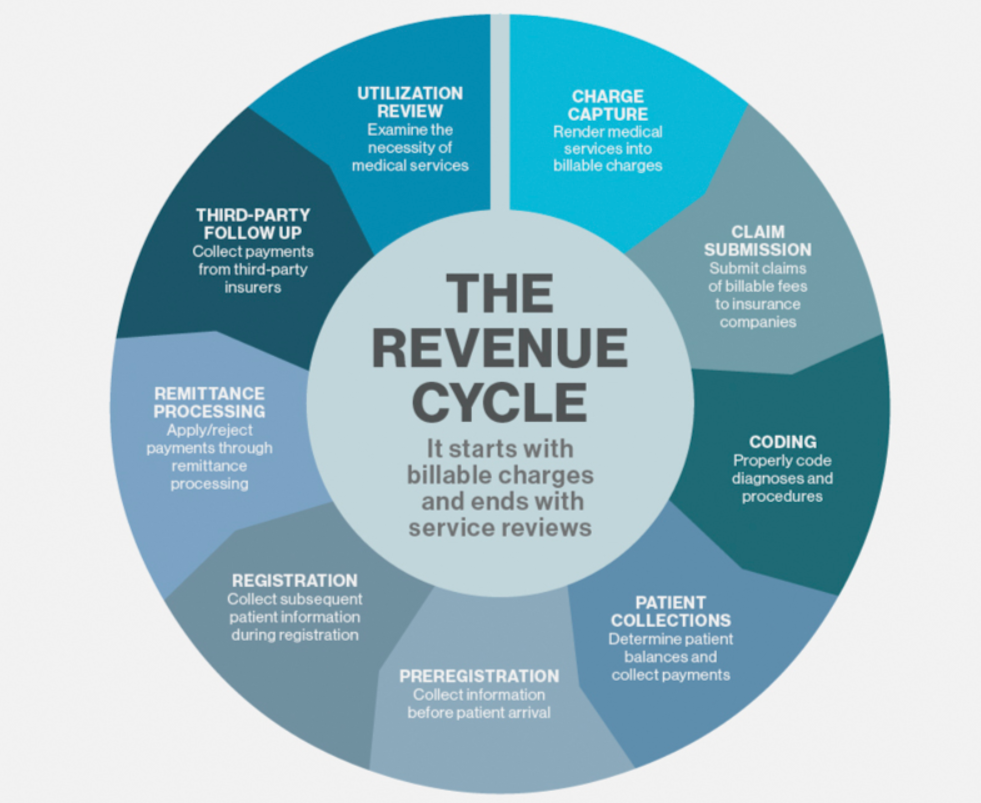
 As the possible repeal of the Affordable Care Act (ACA) becomes a reality, the need for revenue cycle management is absolutely critical. You may be asking yourself what a revenue cycle actually is, especially as it pertains to the business world. The revenue cycle is the crucial process that efficiently and accurately captures the revenue of any organization, regardless of size, from a singular stand-alone doctor physicians practice to a hospital network with more than 10 locations.
As the possible repeal of the Affordable Care Act (ACA) becomes a reality, the need for revenue cycle management is absolutely critical. You may be asking yourself what a revenue cycle actually is, especially as it pertains to the business world. The revenue cycle is the crucial process that efficiently and accurately captures the revenue of any organization, regardless of size, from a singular stand-alone doctor physicians practice to a hospital network with more than 10 locations.
A revenue cycle consists of “all administrative and clinical functions that contribute to the capture, management, and collection of patient service revenue,” describes the Healthcare Financial Management Association. Experts all agree that grave errors discovered in revenue cycles are giving the entire medical industry a headache, as far as federal and state oversight and the production of reports for the government and financial world are concerned.
With mass uncertainty over the fate of the ACA, both patients and healthcare professionals have a reason for concern. The effect on patients would be the very real chance of losing medical coverage and an exponential increase in out-of-pocket health care costs, even if patients do have coverage. On the provider side, health care professionals could sustain dollar losses in the millions because patients cannot afford treatment or they do not pay their medical bills; this, in turn, causes a very obvious increase in accounts receivable (A/R).
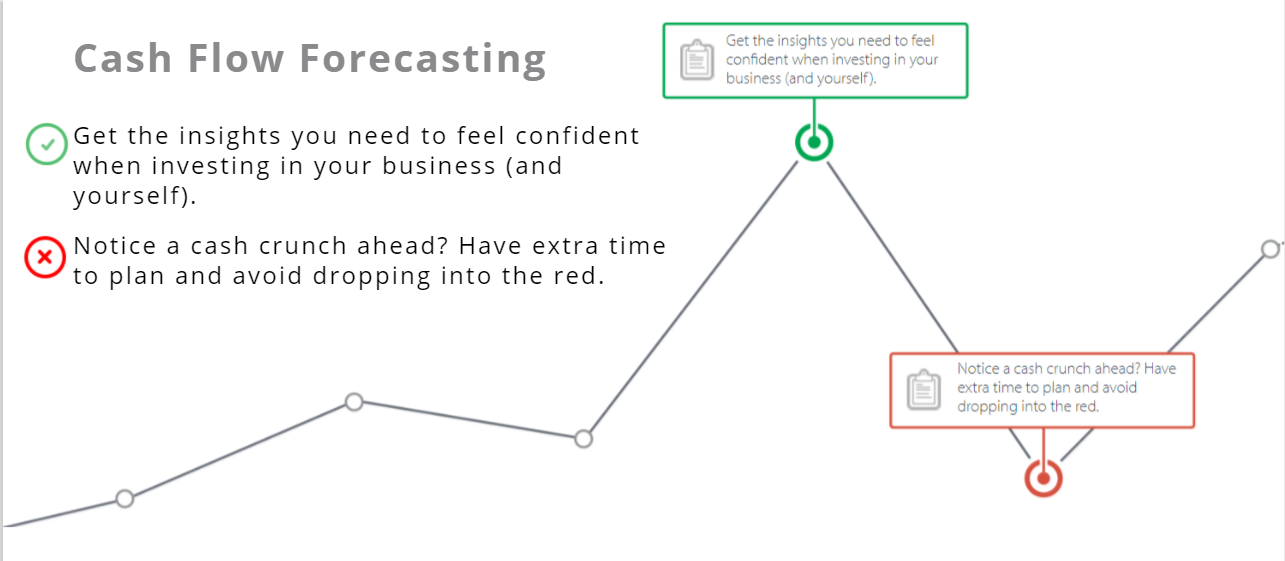
To make matters worse, medical practices, medical groups, healthcare systems and hospitals are targeted by an October 2016 brand new payment model that must be used for patients. Tucked into the final rule for the Medicare Access and Children’s Health Insurance Program Reauthorization Act of 2015 (MACRA), this new standard payment model is outlined. We are now realizing that a serious repercussion of its enactment is large decreases in cash flow.
The medical community is also still suffering to stay effective as it witnesses increasing oversight, more competition and an increase in operational costs, all of which lead to less cash. As you can probably imagine, myriad mistakes and errors, usually revolving around the very revenue cycle process and cash flow, are also rampant.
Improving Revenue Cycle Management in 5 Steps
The strength of any organization’s revenue cycle has to be very robust as it will, on a case-by-case basis because most businesses are unique, be heavily relied upon for achieving an organization’s goals. Case-by-case assessments of revenue cycles will take the following into consideration:
- Compliance Programs
- Technology
- Payer Relationships
- Employee Function
- Reimbursement Cycle
At ProBooks, we have identified 5 steps that can evaluate the above factors, while assisting in the improvement of a revenue cycle and its corresponding management. Let’s take a look at these steps which will enormously affect cash flow- they are:
- Benchmark Billing System Success
- Collection Rate Improvement via Shortened Billing Cycles
- Accountability of Employees & Defining Staff Responsibilities
- Switching Focus to the Net Collection Rate
- Technology Integration
Benchmark Billing System Success
Hospitals are scrambling to meet billing reimbursement standards for their industry. Defining the parameters of standard health care timelines is essential. In order to do this, you will need to collect data on individual payers and standard accounts receivable (A/R) days. This data will be used when you revisit overdue accounts and try to understand collection times. Guidelines need to be developed and put to use; doing so means that you will need the following:
- Where is the location of your business?
- How large is your organization?
- What is the relationship between Medicare/ Medicaid and reimbursement?
- Who is the payer?
Benchmarking data is important when a business wants to highlight how it compares to its peers in the marketplace of health systems and other hospitals within the same niche and geography. A comparison will indicate where and what a business’ inefficiencies are…areas where a business is lacking the need to be focused upon. A comparison and its data will help the business prepare for meticulous scrutiny from state and federal oversight boards- this streamlines the cycle process and alerts management of potentially fraudulent activity.
Collection Rate Improvement via Shortened Billing Cycles
Before billing cycle use, potential liability issues and insurance coverage should be reviewed by a medical group and described, in tandem, to patients. This means communication is key. Patients should know, in advance of a medical procedure or doctor visit, their spend so they are not shocked by a particularly large invoice that needs to be paid out-of-pocket.
Be careful with the topic of collecting by addressing billing facts or concerns immediately; remember that as more and more time goes by, the chance of a payer remitting payment decreases and less profit and higher losses (sometimes in the millions) occur. A common solution for such a conundrum is to focus on the following:
- Denial Reduction
- Only Allowing for Invoices to be Paid in Full
- Disallowing Payment Plans or Payment Installments
- Lessening the Volume of Written Off A/R Accounts
Accountability of Employees & Defining Staff Responsibilities
Clarifying each staff member’s job duties can make holding an employee accountable much easier. This is very helpful for problems surrounding follow-up and incongruity, especially when a business’ revenue cycle is in the picture. This task of making employees accountable can be difficult though- sometimes there are simply too many overlapping contributing factors.
The Management Approach
Businesses have been known to utilize a crisis management method in the event that there is a division of staff responsibilities or some other types of issues. Without clear-cut job responsibilities, there is a huge obstacle on the path to a successful business because revenue cycle process management is compromised. A compromised system that is not streamlined will get you your company nowhere in that it results in an improperly designed and implemented system cycle, poor management, and subpar follow-up- all of which contribute to subpar cash flow and decreased profit. The flipside method could be labeled the proactive approach and that approach focuses on a holistic solution that takes all facets of the business into account.
Checks and Balances
The mechanism of checks and balances is inherent to a business’ billing team and will assist in the rectification of errors while holding employees accountable. Contained in this system is the clear structure of company roles that advocate a fluid structure among revenue cycle stages. When combined with solid management oversight, a business can rest easy knowing that staff members are not operating autonomously.
Staff Training
Less than adequate training for employees usually leads to fines and coding discrepancies. Fulfilling requirements, such as those associated with the legally binding CMS 60-day refund rule and 501(r) charity reporting guidelines. As a scope broadens, more focus and effort must be put into remaining compliant. Staff members need to obtain accurate data on patient information and code invoices properly so bills are error-free and collectible. Inaccurate billing increases the probability of denials and contributes to longer than usual collection time. When coding is improper, a business can be faced with accidental billing fraud and heavy fines.
Vendor Relationships
The health of the relationship between vendors in the revenue cycle and a health care network’s billing department can be frustrating, to begin with- this is especially notable when there is a question which party should be accountable. The definition of how a business should interact should be clearcut A successful revenue cycle depends on a defined relationship between a vendor and its point of contact. This will assist in the obtaining and exchanging of information between parties. Try giving certain monitoring tools a chance- those tools are designed to maintain and enhance communication methods.
Additional Benefits
Streamlining a revenue cycle almost guarantees increased cash flow but it also has other benefits. These benefits would be an insight into the division of duties, on-target job descriptions, and more training, just to name a few. All-in-all, everyone in the business will have reduced stress and experience less conflict.
Switching Focus to the Net Collection Rate
Although accounts receivable A/R is an important performance indicator, it will not present a full picture. Shifting focus to the net collection rate gives businesses a more accurate answer as to whether they are collecting funds for a full amount due.
A/R will provide insight into the time currently needed to move an account from posting to payment. Net collection rates illustrate the performance of an organization as it pertains to the collection of funds that are invoiced. Tunnel vision that focuses solely on A/R can be very risky and sometimes disastrous because an unjustly write-off may be designed and implemented to satisfy target dates. Organizations that choose to instead focus on net collection rates will be helping themselves ensure that almost all debt collection methods are tried before A/R accounts are written off- sometimes this approach will allow for a company to collect more.
Net Collection Rate
The net collection rate is a telling percentage and represents the reimbursement rate that a business has achieved based on allowances and contractual obligations; a net collection rate will identify lost revenue due to:
- Filings that are untimely and unpredictable in nature
- Adjustments made that are not part of a contract
- Debt that is uncollectible
How to Calculate Your Net Collection Rate
Start by dividing payments (net of credits) by charges (net of approved contractual adjustments) for the time period that you want to monitor. Then multiply by 100 to get the percentage value. Payments need to match with their originating charges for the most accurate calculations, so you might want to number these by “date of service” instead of “date of post.” If your practice management system can’t match payments with their originating charges, the practice should calculate this using aged data, typically from six months back, to ensure a majority of the claims used for the calculation have had enough time to clear.

To improve a net collection rate, try increasing the frequency of your communication with payers and scrutinizing payer contracts. It might be the case that your payers are under-reimbursing or denying too many claims. A stricter follow-up process can also remedy issues with a business’ payers.
Work with Existing Technology
Healthcare professionals must understand that there is a lag in noticing a higher cash flow after even significant changes in their revenue management data system‘s cycle; we can attribute that fact to the two following factors:
- Cycle systems that were set up improperly
- Employees running cycle systems improperly
These factors are overcome by revising and updating revenue cycle functionality discovered in operational processes. By the same token, cycle systems can also be altered and modified if improved operations are achieved; taking note of what is being analyzed because changes need to be addressed with a solution. As an example, work queue timeframes are allowed to be modified so accounts are not mislabeled past due because of timeframe issues.
Conclusion
There is no real way to navigate the healthcare environment that is not challenging. You will, most likely, require the skill that only an expert accountant or CPA can offer if you want to operate a successful business in this atmosphere. Successful healthcare revenue cycle management strategies focus on front-end tasks to help claims move along. Many errors occur in the first stages of a patient’s account and these issues can carry through the revenue cycle to disrupt claims reimbursement. If you would like to hear more about increasing the probability of your business being successful, or how you can reach cash flow dollar goals with your revenue cycle management process, contact ProBooks.
accountant or CPA can offer if you want to operate a successful business in this atmosphere. Successful healthcare revenue cycle management strategies focus on front-end tasks to help claims move along. Many errors occur in the first stages of a patient’s account and these issues can carry through the revenue cycle to disrupt claims reimbursement. If you would like to hear more about increasing the probability of your business being successful, or how you can reach cash flow dollar goals with your revenue cycle management process, contact ProBooks.